The sterile field in dental surgery
Dental implantology, cross infections and aseptic technique
In the exercise of the dental profession, we are exposed daily to a huge quantity of viruses and bacteria that can cause infections. This is an even more significant issue during surgical (and dental implant) operations that involve incisions of the tissues and more invasive action.
It is important to remember that all the surfaces that surround us are covered with microorganisms which can contaminate the surgical wound during surgery and cause infection, with negative consequences both for the success of the operation and for the health of the patient. These microorganisms can also cause various cross infections between patients, and from patient to doctor, and vice versa.
With the invention and the use of dental implants, aseptic techniques are gradually being used in the field of dentistry. Today, thanks to an exhaustive biosafety protocol and the creation of a sterile field, it’s possible to manage the risk of infection and reduce it to a minimum.
Many intra- and post-operative complications could be avoided with the use of a correct aseptic technique.
Organising spaces and instruments, following the correct hand scrub, gown and glove procedure and adequately preparing the surgical field will not only prevent infection of the surgical wound, it will also protect patients and operators from cross infection.
How to prepare the operating room for dental surgery
When performing the surgery, we will try to have the lowest possible number of microorganisms in the environment surrounding the patient. When preparing for a surgery, we will divide the room into two areas:
STERILE AREA: This is where the sterile material and scrub nurses will be. There will also be the chair for the patient and the sterile drapes. There will be a table covered with another sterile drape where we will put the surgical instruments and the necessary items for the surgery. The staff working in this area must have performed a surgical hand scrub. Despite the use of sterile gloves, it is essential that hands are washed properly.
Normally there will be a sterile services assistant, although in larger practices there may be a scrub nurse. The sterile services assistant is responsible for placing the material on the surgical table and laying the surgical drapes. The scrub nurse must have an excellent understanding with the surgeon, since they will supply the surgical instruments in the surgeon’s usual order, as well as the dental drills and other equipment needed for the surgery.
NON-STERILE AREA: this area is separated with an imaginary line. The non-sterile staff and circulant nurses will be in this area. The role of the non-sterile staff is to help the sterile staff to wash their hands and don the surgical gown. They are also responsible for opening material in the surgical field and providing the patient with the scrub cap and shoes for the surgical field, and for providing the chlorhexidine for the mouthwash.
In addition, for the surgery to be carried out in the best possible conditions, the room chosen for surgery:
- must have been completely cleaned with disinfectant beforehand, and countertops should be as clear as possible
- should be as far away from patient traffic and non-surgical staff as possible
- must have the doors closed in order to prevent aerosol from circulating, which could contaminate the surgical wound
PPE in dental surgery
Before entering the room, staff must don scrub cap, scrub shoes and mask. The mask should be placed snugly on the bridge of the nose with safety glasses or safety screen on top.
Before the surgery, it is very important that all the necessary material has already been prepared. Written protocols will help us to ensure that nothing is forgotten. In addition to all the required items in terms of equipment, surgical instruments and biomaterials, we need to have all the disposable materials that will be used for treatment.
As well as the sterile drapes, protective covers for hoses, irrigation tubes, gowns or caps, there are also sterile kits which basically contain everything you need so that you don’t forget anything. All the bagged material will be placed in the non-sterile area.
How to wash your hands for surgical purposes
Even if we will be using gloves to prevent contamination, we need to take into account that gloves are only effective for a limited amount of time. Gloves made from latex or nitrile are best in terms of quality and length of time they are effective for, while vinyl gloves have the most faults reported due to their structure, being the ones that break the most.
There are four types of hand washing:
1. Hygienic washing
This is done with neutral soap and must be carried out: – before starting the examination – between one patient and the next – after going to the bathroom – before putting on the gloves – after touching dirty or contaminated material.
Lather soap and scrub the entirety of the hands and spaces between the fingers, completely removing any dirt in the nails, and rinsing thoroughly. After drying the hands with a disposable paper hand-drying towel, turn the tap off with a sheet of paper towel.
2. Antiseptic washing
Antiseptic washing is made up of two stages. In the first stage, we carry out hygienic washing as previously described, and in the second stage we use a water-based alcohol disinfectant to remove dirt, organic and microbial material, both transient and resident.
3. Washing with alcohol-based solution
This is carried out in locations where there is no water tap to carry out a standard hand wash. Scrub vigorously with the solution for 30 seconds. If your hands dry before this time then add more solution.
4. Surgical washing
This is carried out before surgery. It involves removing both transient and resident flora. To perform the surgical washing procedure, you need a tap that can be operated using the elbow, knee or foot, a disposable sponge, an antiseptic scrub with either a povidone iodine or chlorhexidine base (studies show that chlorhexidine is more effective), and two sterile towels. The ideal would be to use single-use, impregnated sponges.
Donning the gloves and the sterile gown
After washing the hands, don the gown. Surgical gowns are folded at the back, so that the non-sterile part (touching the body) is the first part we can touch. There are two ways of donning the gown:
- Putting it on yourself: With two fingers, open the gown and put the arms through the sleeves. A non-sterile assistant will do up the tie at the back, as this area is considered to be non-sterile.
- Getting someone to help you: The sterile services assistant, already dressed, will open the gown up to the other person, to help them put it on. The circulant assistant will do up the tie at the back.
Go into the surgical area with arms pointing upwards. The non-sterile assistant will have opened up a surgical drape for us, as well as the sterile gown. The surgical gown comes pre-folded outwards, to make it easier to put it on yourself.
Put your arms through the gown without shaking it on and get the assistant to do up the tie at the back. The area at the back is considered non-sterile. The assistant will then open the gloves for us, leaving the internal packaging exposed. We will open it out like a book, leaving the gloves uncovered. With the thumb and index finger, in one swift movement, slide in the hand – taking the edge of the glove by the folded cuff and insert the hand, leaving the cuff turned down over the hand. Put this hand into the fold of the other glove in order to grasp it, then insert the other hand into the glove with one swift movement.
At this point, you must only touch things that are sterile. This is extremely important. You cannot do things like adjust your mask or touch any surfaces that have not been covered. If you do, you will need to put on new gloves.
How to prepare the sterile surgical field
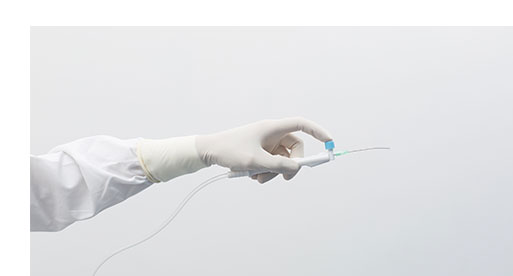
Place the sterile drape over the surface you will be working on. The non-sterile assistant will open up the material. Place the material in the sterile field. Without touching the suction device, insert the sterile surgical cannula.
Put the protective covers on the hoses without touching anything that isn’t sterile. After doing this you cannot put it back on the normal bracket, as the suction device will become contaminated. Seal the top part with an adhesive so it does not fall.
In order to cover the areas of normal use, such as light handles and implant drills, there are some transparent adhesive sterile films which will help us.
Place the sterile irrigation tube in the contra-angle and the non-sterile assistant will connect it to the saline solution and implant drill. In the event that an external irrigation tube is used, it is important to know that the saline will be contaminated the first time the syringe is inserted to absorb the saline. Saline dispensers are available which provide a continuous irrigation, without contaminating the saline each time you inject it.
It is now time to bring the patient into the sterile field. Before coming into the room, the non-sterile assistant will provide the patient with scrub shoes, gown and scrub cap. The patient should already be dressed when they come in.
Inside the room, the patient will be given a 0.12% chlorhexidine mouthwash to rinse for a period of 60 seconds. Next, the peri-oral area will be cleaned with Chlorhexidine or povidone iodine. To do this, put the solution on the gauze and carry out extrinsic movements, from the lips to the peripheral area.
Positioning the sterile drape on the patient
Today, thanks to the new products available on the market, patients can be draped more safely and in a few simple movements. Traditional procedures have been replaced with disposable sterile drapes. Fenestrated drapes with adhesive are available, which stick firmly onto the area where you are going to work. The ideal solution would be to use a U-shaped cutout adhesive sterile drape and fix it with another drape on top of the patient’s head.
Surgical drapes with a window are also available, which have a transparent window over the eyes. This allows patients to see what is going on around them, preventing them from getting anxious.
During surgery, it is very important not to touch anything that is not covered with sterile material. Doors must be closed, and it is better to avoid staff coming in from the outside. All staff in the room must wear scrub shoes, mask and scrub cap.
After completing surgery, all the contaminated drapes and gowns should be removed. Scalpels and sharp materials should go in the corresponding containers. The mask should be the last item you remove. First, undo the bottom tie, then undo the top one. If you do it the other way around, the mask will fall backwards and the contaminated part will touch the neck.
All the autoclavable material will undergo a thorough decontamination, washing and sterilisation process. The room will be aired and both the furniture and the suction tubes will then be meticulously cleaned.
Safety, quality and success in dental surgery: the sterile field
All of these actions will make it easier to perform surgery in the proper and correct way, preventing the biomaterials used from being contaminated before entering the body, causing the surgery to fail.
Moreover, we are protecting the patient from any potential contamination of the surgical wound. The bacteria that are not found in the oral environment in normal conditions could infect the surgical wound and cause severe postoperative complications, which could lead to serious problems.
As well as protecting the patient, we are also protecting ourselves by wearing the appropriate attire, and by having most surfaces in the room covered, we are protecting any other patients who will be sitting in the chair later.